Recognizing the Signs: How to Spot a Calcium Deficiency
Many individuals may unknowingly experience low calcium levels, often dismissing the early, subtle signs. It’s crucial to understand that what happens when your calcium is low can manifest in ways that are easily overlooked. Common symptoms include muscle cramps, which can range from mild twitches to more painful spasms, often occurring in the legs, feet, or hands. Another frequently reported symptom is persistent fatigue, a general feeling of being tired and lacking energy, even after sufficient rest. This isn’t just ordinary tiredness; it’s a persistent drain that can affect daily activities. Additionally, individuals with low calcium may experience tingling sensations or numbness, typically in the hands, feet, and around the mouth, caused by the impact of reduced calcium on nerve function. Brittle nails, which are prone to breaking, chipping, or peeling, can also indicate a deficiency. These signs, often viewed as minor inconveniences, should not be ignored. Early detection is essential because what happens when your calcium is low can lead to more serious health complications if left unaddressed. Understanding the importance of recognizing these subtle cues empowers individuals to take proactive steps toward maintaining healthy calcium levels and avoiding more severe health issues. The interconnectedness of the body’s systems means a deficiency in one area, such as calcium, can have a domino effect impacting different parts of your well-being. These seemingly small symptoms should prompt further investigation into potential nutritional deficiencies and underscore the significance of maintaining a balanced diet and regular health check-ups. When one understands the consequences of ignoring these early indicators, they are more likely to take the necessary steps to preserve their overall health. Don’t dismiss these subtle signs; they could be your body’s way of signaling that it needs more calcium, because what happens when your calcium is low can have a significant impact on your overall health and well-being.
The Domino Effect: What Happens to Your Body When Calcium Is Low
Calcium is not merely a component of strong bones; it’s a vital mineral that orchestrates a myriad of bodily functions. When the body experiences low calcium levels, it sets off a chain reaction impacting several crucial systems. One of the most significant consequences of low calcium relates to bone health. The skeletal system serves as the body’s calcium reservoir, and when dietary intake is insufficient, the body begins to draw calcium from the bones to maintain normal blood levels. This process, over time, leads to a decrease in bone density, increasing the risk of developing osteopenia and ultimately osteoporosis, a condition characterized by weak and brittle bones prone to fractures. This is a serious consideration regarding what happens when your calcium is low. Beyond bone health, calcium plays a key role in muscle function. It’s essential for muscle contraction and relaxation. Consequently, a deficiency can manifest as muscle cramps, spasms, and general weakness. These symptoms can range from mild discomfort to more severe limitations in mobility, underscoring the importance of maintaining adequate calcium intake to support muscle health. Nerve transmission is also highly dependent on calcium. Nerves use calcium to send signals throughout the body. Low calcium disrupts this communication system, leading to symptoms such as tingling and numbness, especially in the hands and feet. These neurological symptoms can sometimes be subtle and go unnoticed, yet they are indicators of a systemic calcium deficiency and contribute to the understanding of what happens when your calcium is low. Another crucial role of calcium is in blood clotting. When an injury occurs, calcium is one of the elements necessary to initiate the coagulation cascade, a process that stops bleeding. What happens when your calcium is low in this context? If calcium levels are low, the body’s ability to form blood clots can be compromised. It is worth noting that while calcium deficiency is not the only cause of clotting problems, it contributes to this important process, further highlighting the wide-ranging impact of this essential mineral. The consequences of low calcium go beyond easily discernible symptoms. Because calcium is involved in so many fundamental processes, a deficiency can impact overall health and well-being. Therefore, paying close attention to the subtle warning signs and working to maintain adequate calcium levels is crucial for preventing the domino effect of health issues that can arise when calcium levels are compromised. Recognizing what happens when your calcium is low provides a critical insight into how important it is to proactively manage calcium intake.
Bone Density and Low Calcium: The Long-Term Consequences
The repercussions of persistently low calcium levels extend far beyond immediate discomfort, significantly impacting long-term bone health. A chronic deficiency can pave the way for serious conditions like osteoporosis, a disease characterized by weakened and brittle bones. Individuals with osteoporosis face an alarmingly heightened risk of fractures, often from minor falls or even everyday activities. This vulnerability is particularly concerning for older adults, whose bone density naturally declines with age, and post-menopausal women due to hormonal changes that accelerate bone loss. Understanding bone remodeling is crucial to grasping why this occurs. Bone remodeling is a continuous process where old bone tissue is broken down and replaced with new tissue. This process requires a consistent supply of calcium. When calcium intake is insufficient, the breakdown of old bone outpaces the formation of new bone, leading to a gradual decrease in bone density. What happens when your calcium is low is that the body starts taking calcium from the bones to maintain other crucial functions which further weakens the skeletal structure. This imbalance eventually leads to osteopenia, the precursor to osteoporosis, marked by lower than normal bone density. It is important to recognize that the effects of low calcium on bone health is not an immediate issue, it is gradual and the long term results can be detrimental. It’s a slow decline that might go unnoticed until a fracture occurs. The decrease in bone mass from low calcium levels can lead to a significant loss of height and changes in posture, making people more susceptible to falls and fractures of the hip, spine, and wrist. What happens when your calcium is low is that it impairs the normal bone remodeling cycle. This slow progression of bone damage makes early detection and intervention all the more critical. A lack of adequate calcium over time results in bones that are increasingly porous and susceptible to breakage, severely compromising mobility, independence, and overall quality of life. Therefore, understanding that maintaining healthy calcium levels is essential for robust and durable bone structure throughout life. The consequences of ignoring a calcium deficiency are not just about immediate discomfort, but they affect long term well being. What happens when your calcium is low is that it not only diminishes bone density but can also lead to a cascade of skeletal health problems. Regular monitoring and intervention to maintain proper calcium levels are paramount for preserving bone integrity and preventing devastating outcomes. In essence, the impact of low calcium on bones is a clear demonstration of how this seemingly simple nutrient is vital for ensuring lifelong health and mobility.
How To Improve Calcium Levels Through Diet
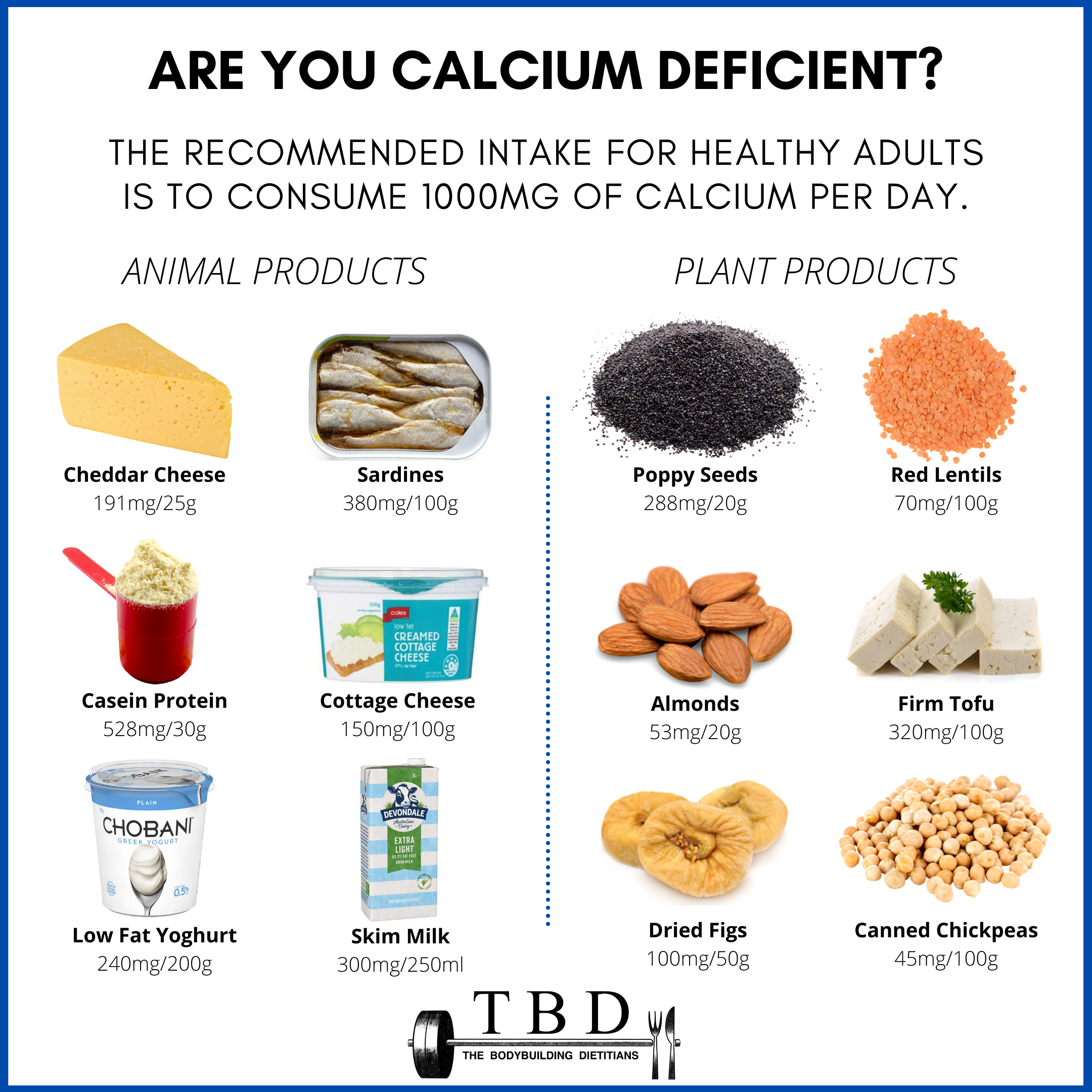
Diet plays a pivotal role in maintaining healthy calcium levels. Understanding which foods are rich in calcium and incorporating them into daily meals is a significant step in preventing what happens when your calcium is low. Dairy products, renowned for their calcium content, are excellent choices. Milk, cheese, and yogurt, are readily accessible and versatile ingredients that can be easily included in various meals or enjoyed as snacks. However, dairy is not the only source of calcium. Leafy green vegetables such as kale, collard greens, and spinach are surprisingly good sources of calcium. These can be included in salads, soups, smoothies, or as a side dish, adding not only calcium but also other essential vitamins and minerals to your diet. Fortified foods also play a crucial role in boosting calcium intake. Many plant-based milk alternatives, cereals, and orange juices are fortified with calcium, making them an excellent option for those who might avoid dairy products or struggle to get enough calcium from other sources. Some types of fish, like canned sardines and salmon, also provide calcium, and are good choices, especially when the bones are consumed. These options can be included in your weekly diet to contribute to your overall calcium intake. Meal planning can be beneficial to make sure you are eating enough calcium-rich foods. For breakfast, consider yogurt with fortified cereal. For lunch, a salad with leafy greens and cheese would be excellent. As a snack, almonds are a good option, though they should be eaten in moderation due to the high caloric content. Dinner could include fish with a side of cooked collard greens. These are just a few examples of how to integrate calcium-rich foods into your meals. Consistent intake of these foods is more beneficial than relying solely on supplements. It is important to build a routine of consuming calcium-rich foods in your daily life. What happens when your calcium is low is often the result of diet neglect over long periods. Relying on supplementation alone, while sometimes necessary, shouldn’t be the first action, as food provides other vital nutrients and the body can assimilate calcium better from natural sources. Developing healthy eating habits and focusing on diverse calcium-rich foods can effectively address and prevent low calcium levels. Making informed dietary choices and preparing well-balanced meals is an effective strategy to address what happens when your calcium is low and help maintain your bone health, muscle function, and overall well-being, over the long-term. When addressing calcium levels through diet, it’s not just about the quantity, but the consistent effort to incorporate a variety of calcium-rich foods. By building habits around calcium rich foods, readers are empowered to take control over their health and mitigate the risks associated with calcium deficiency.
Beyond Diet: The Role of Vitamin D in Calcium Absorption
Vitamin D plays a crucial, yet often underappreciated, role in the intricate dance of calcium absorption within the human body. While consuming calcium-rich foods is a fundamental step in maintaining healthy levels, the body’s ability to actually utilize this essential mineral hinges significantly on the presence of adequate Vitamin D. Think of Vitamin D as the key that unlocks the door, allowing calcium to move from the digestive system into the bloodstream, and ultimately, into the bones and other tissues that require it. Without sufficient Vitamin D, the body struggles to absorb calcium effectively, even when dietary intake is optimal. This can lead to a scenario where, despite consuming calcium-rich foods, individuals still experience the detrimental effects of low calcium. Natural sunlight exposure serves as a primary source of Vitamin D, as the body synthesizes this vital nutrient when exposed to ultraviolet B (UVB) rays. However, factors such as geographical location, time of year, and skin pigmentation can affect the amount of Vitamin D produced through sun exposure. Dietary sources offer an alternative, though sometimes insufficient, route to obtain Vitamin D. Fatty fish like salmon, mackerel, and tuna are excellent sources, and fortified foods such as milk, some cereals, and plant-based milk alternatives are often enhanced with Vitamin D.
What happens when your calcium is low is that the body will struggle even if you have an adequate calcium intake. It is crucial to understand that a Vitamin D deficiency can essentially negate the benefits of even the most diligent calcium intake efforts. If Vitamin D levels are insufficient, the body will not be able to absorb calcium effectively, increasing the risk of low calcium-related problems, like brittle bones and muscle weakness. To ensure optimal calcium absorption and utilization, it is important to understand your Vitamin D status. A simple blood test, specifically a 25-hydroxyvitamin D test, can determine whether your Vitamin D levels are adequate. Healthcare providers generally recommend vitamin D levels to be between 30 and 50 ng/mL, but it’s critical to discuss your specific needs with your physician, as optimal levels can vary depending on individual circumstances and health conditions. Regular monitoring can identify any existing deficiency and inform necessary dietary or supplement adjustments to maintain optimal calcium absorption. Therefore, while diet is a cornerstone of maintaining adequate calcium levels, do not underestimate the equally important need for sufficient vitamin D. The body needs both to operate effectively, and insufficient levels of either can result in health issues.
When Diet Isn’t Enough: Exploring Calcium Supplements
While a diet rich in calcium is the cornerstone of maintaining healthy levels, there are instances when dietary intake alone may fall short. Certain individuals, due to specific health conditions, age, or dietary restrictions, might require additional support in the form of calcium supplements. Understanding the nuances of supplementation is essential for ensuring safe and effective use. Several types of calcium supplements are available, each with distinct characteristics. Calcium carbonate is a commonly found option, known for its high calcium content and affordability. However, it requires stomach acid for optimal absorption, making it most effective when taken with food. On the other hand, calcium citrate is more readily absorbed, even on an empty stomach, making it a preferable choice for individuals with digestive issues or those taking medications that reduce stomach acid. The choice between these options, and others such as calcium lactate or gluconate, should be made with guidance from a healthcare professional to address unique needs and any underlying health issues. It is crucial to be aware of potential side effects associated with calcium supplementation. Common side effects can include gas, bloating, and constipation, particularly with calcium carbonate. High doses of calcium supplements may also interact with certain medications, such as some antibiotics, diuretics, and thyroid hormones. Furthermore, excessive calcium intake from supplements can sometimes lead to hypercalcemia, a condition where there is too much calcium in the blood, potentially causing kidney problems and other health issues. It’s important to remember that more is not always better. What happens when your calcium is low, can be complex, and blindly taking supplements without proper guidance may not address the root cause of deficiency or be the most efficient approach. Rather than self-prescribing supplements, a healthcare provider is best equipped to assess individual needs, determine if supplementation is indeed necessary, and prescribe the correct dosage. They will also take into consideration any existing health conditions and medications being taken to minimize the risk of side effects and interactions. When considering supplementation, it is vital to have an understanding of how much calcium one needs daily, which varies based on age, gender, and other factors. The recommended daily intake is different for children, teenagers, adults, and pregnant or breastfeeding women. This makes the personalized guidance from a healthcare professional even more critical to make well-informed choices regarding supplementation. Ultimately, calcium supplements should be seen as an adjunct to a healthy diet, not a replacement. Working with a doctor or registered dietitian to create a tailored approach to nutrition and supplementation offers the best pathway to maintain appropriate calcium levels.
Taking Action: How to Consult a Doctor About Calcium Deficiency
Seeking professional medical advice is crucial for the proper diagnosis and treatment of low calcium levels. A doctor can assess individual needs and provide personalized recommendations to address what happens when your calcium is low. The first step typically involves a consultation where a healthcare provider will inquire about your medical history, including any symptoms you might be experiencing. It’s important to be prepared to discuss any subtle signs such as muscle cramps, fatigue, tingling sensations, or brittle nails, as these might indicate a potential calcium deficiency. To confirm a diagnosis, a doctor will likely order specific tests. A simple blood test can accurately measure your current calcium levels. However, this is not always sufficient, as blood levels may not reflect the overall calcium store in the body. For a more comprehensive view, a bone density test may also be recommended. This test, often called a DEXA scan, measures the mineral content of your bones, providing insight into bone health and detecting conditions like osteopenia or osteoporosis, which are directly linked to what happens when your calcium is low over a prolonged period. This is particularly important for older adults and post-menopausal women who are at higher risk of bone loss. The test results will help determine whether you have a deficiency and to what extent it has impacted your health. The frequency of these tests might vary based on age, gender, medical history, and risk factors for low calcium. For instance, individuals with a family history of osteoporosis may require more frequent bone density tests. The treatment plan will be customized based on your unique needs. It’s important to recognize that calcium requirements differ across individuals. Factors such as age, gender, overall health, and lifestyle play significant roles. A doctor will help establish the right calcium intake level. It’s important to engage with your doctor regarding your specific calcium needs and concerns about what happens when your calcium is low, asking questions to clarify any doubts. This active role is essential for effectively managing your calcium levels. If supplementation is needed, the doctor can recommend the right type and dosage based on your needs. Furthermore, they can also educate you on the importance of vitamin D for calcium absorption and offer advice on incorporating Vitamin D through sunlight exposure or supplementation as needed. Regular follow-ups with your doctor allow monitoring of the effectiveness of the treatment plan and making any necessary adjustments. Don’t hesitate to communicate all of your symptoms or concerns. Early intervention is crucial in managing the impact of low calcium levels and preventing serious long-term health complications. Always prioritize a personalized approach that takes into account your health profile and circumstances to manage what happens when your calcium is low.
Maintaining Healthy Calcium Levels: A Lifestyle Approach
Maintaining healthy calcium levels is not a singular action but rather an ongoing commitment to a balanced lifestyle. It involves a multifaceted approach combining a diet rich in calcium, adequate Vitamin D intake, regular physical activity, and consistent medical check-ups. Understanding what happens when your calcium is low underscores the importance of this holistic strategy. Ensuring adequate calcium intake is not just about consuming calcium-rich foods; it also entails understanding how your body absorbs and utilizes this vital mineral. A diet abundant in dairy products, leafy greens, fortified foods, and certain types of fish provides a strong foundation. However, it’s equally crucial to ensure you are getting enough Vitamin D, either through sunlight exposure or Vitamin D-rich foods such as fatty fish and fortified products. Vitamin D significantly enhances the absorption of calcium, making both equally important for bone health, muscle function, nerve transmission and blood clotting. Regular physical activity plays a crucial role in maintaining bone density. Weight-bearing exercises, in particular, can stimulate bone remodeling and help the body maintain bone strength. The synergy between calcium intake, Vitamin D, and exercise creates a powerful defense against bone weakening conditions such as osteoporosis. Furthermore, what happens when your calcium is low can be exacerbated by other lifestyle choices. Therefore, minimizing factors such as excessive alcohol consumption and smoking is crucial for optimal calcium absorption and utilization. Regular check-ups with a doctor are essential to ensure your calcium levels are within the healthy range, especially for those at higher risk. During these visits, healthcare professionals can assess individual calcium needs based on factors such as age, gender, medical history, and perform necessary tests such as blood tests to measure calcium levels, or bone density tests. Moreover, these checkups allow open communication to understand what happens when your calcium is low, based on symptoms you may be experiencing, enabling a quicker response to any developing deficiencies and helping to prevent long term health consequences. In essence, maintaining healthy calcium levels is a continuous process that requires consistent attention to diet, lifestyle, and regular medical care. It is about making a conscious commitment to overall health and well-being to avoid the serious and long lasting implications of what happens when your calcium is low. By adopting a proactive and comprehensive approach, individuals can effectively support their calcium needs and safeguard their long-term health.