Recognizing the Signs of Medial Tibial Stress Syndrome
Correctly identifying the symptoms of lower leg pain is crucial for effective treatment. Medial Tibial Stress Syndrome (MTSS), commonly known as shin splints, is a prevalent condition causing pain along the inner edge of the tibia, the shin bone. Understanding how to know if you have shin splints involves recognizing this characteristic pain location. Many individuals experience pain along the inner aspect of the shin, often feeling a dull ache or sharp pain. This pain frequently intensifies during or after physical activity, particularly activities involving repetitive impact on the legs. Knowing the typical location of shin splint pain is the first step in determining if this condition is the cause of your discomfort. This initial understanding helps differentiate it from other potential issues affecting the lower legs, allowing for targeted self-assessment and appropriate management strategies. Learning how to know if you have shin splints involves paying close attention to the specific nature and location of your pain. Knowing this will allow for earlier diagnosis and intervention, ensuring faster healing and preventing further complications.
Shin splints often manifest as a diffuse, aching pain along the inner border of the tibia. It’s important to differentiate this from sharper, more localized pain that might indicate a stress fracture. While shin splint pain is often described as a dull ache, a stress fracture typically presents with a more intense, pinpoint pain at a specific location along the shin bone. How to know if you have shin splints also involves considering the intensity and nature of your pain. The pain associated with shin splints typically increases with activity and decreases with rest, whereas the pain from a stress fracture may be present even at rest. Understanding these nuances in pain description is vital in making a preliminary self-assessment. The ability to distinguish between the types of pain associated with shin splints versus other conditions, such as stress fractures or compartment syndrome, is key to knowing if further medical evaluation is needed. By carefully noting the location, intensity, and characteristics of your lower leg pain, you can begin to determine whether your symptoms point towards shin splints or a more serious condition. This initial self-assessment will help guide the next steps in your management plan.
To further understand how to know if you have shin splints, consider the gradual onset of symptoms. Shin splints rarely appear suddenly; instead, the pain usually develops gradually over time, often worsening with increased activity levels. This slow progression of symptoms is a key differentiator from conditions like stress fractures, which often have a more acute onset. Paying attention to the gradual development of discomfort, coupled with the location and type of pain, will significantly aid in self-assessment. Remembering that shin splints generally improve with rest is another valuable clue. Finally, self-assessing for shin splints requires recognizing the importance of seeking professional advice when symptoms are severe, persistent, or accompanied by other concerning signs such as swelling or difficulty bearing weight. It’s always crucial to prioritize a proper medical diagnosis for a conclusive answer to “how to know if you have shin splints.”
How to Pinpoint Shin Splint Pain
Understanding the specific characteristics of shin splint pain is crucial when learning how to know if you have shin splints. The pain associated with Medial Tibial Stress Syndrome (MTSS) is typically described as a dull, aching sensation along the inner border of the tibia, the large bone in your lower leg. It’s not usually a sharp, stabbing pain but rather a persistent discomfort that can vary in intensity. This ache is often more noticeable during or immediately following physical activity, such as running, jumping, or even prolonged walking. In the early stages, the pain might subside with rest, but as the condition progresses, it can become more constant and even interfere with daily activities. Pay attention to how the pain responds to activity and rest, as this can help distinguish shin splints from other conditions. The discomfort is not usually concentrated in one specific spot but rather spread out along a section of the shin bone. The pain may also be more pronounced in the lower two-thirds of the tibia, closer to the ankle than the knee, which is significant when considering how to know if you have shin splints. This helps in differentiating from other pain causes located elsewhere in the leg. It’s also important to consider that, unlike a stress fracture, the pain from shin splints is often not localized to a pinpoint area on the bone but rather along the length of it.
To further clarify how to know if you have shin splints, consider how the pain reacts to touch and the absence of severe pain while at rest. Typically, the area along the tibia will be tender to the touch, meaning you’ll experience discomfort when you gently press along the inner shin. However, the pain from shin splints shouldn’t prevent you from being able to bear weight in most cases, though it will be present during weight bearing exercise or activity. This contrasts with a stress fracture, where the pain might be more localized and intense, and bearing weight might be more difficult or impossible. The pain from a stress fracture will often be much more specific and can be pinpointed with a finger as opposed to the general area of shin splint discomfort. Furthermore, pain associated with shin splints tends to increase gradually over time. A sudden onset of severe pain is less typical of shin splints and may indicate another condition, including but not limited to a stress fracture. So, while observing how the pain starts and progresses is critical in understanding how to know if you have shin splints, it is essential to also pay attention to the character of the pain, its location, and its response to touch and rest, all of these factors combined, contribute to a comprehensive self-assessment process to identify shin splints.
Self-Assessment Techniques for Shin Splint Diagnosis
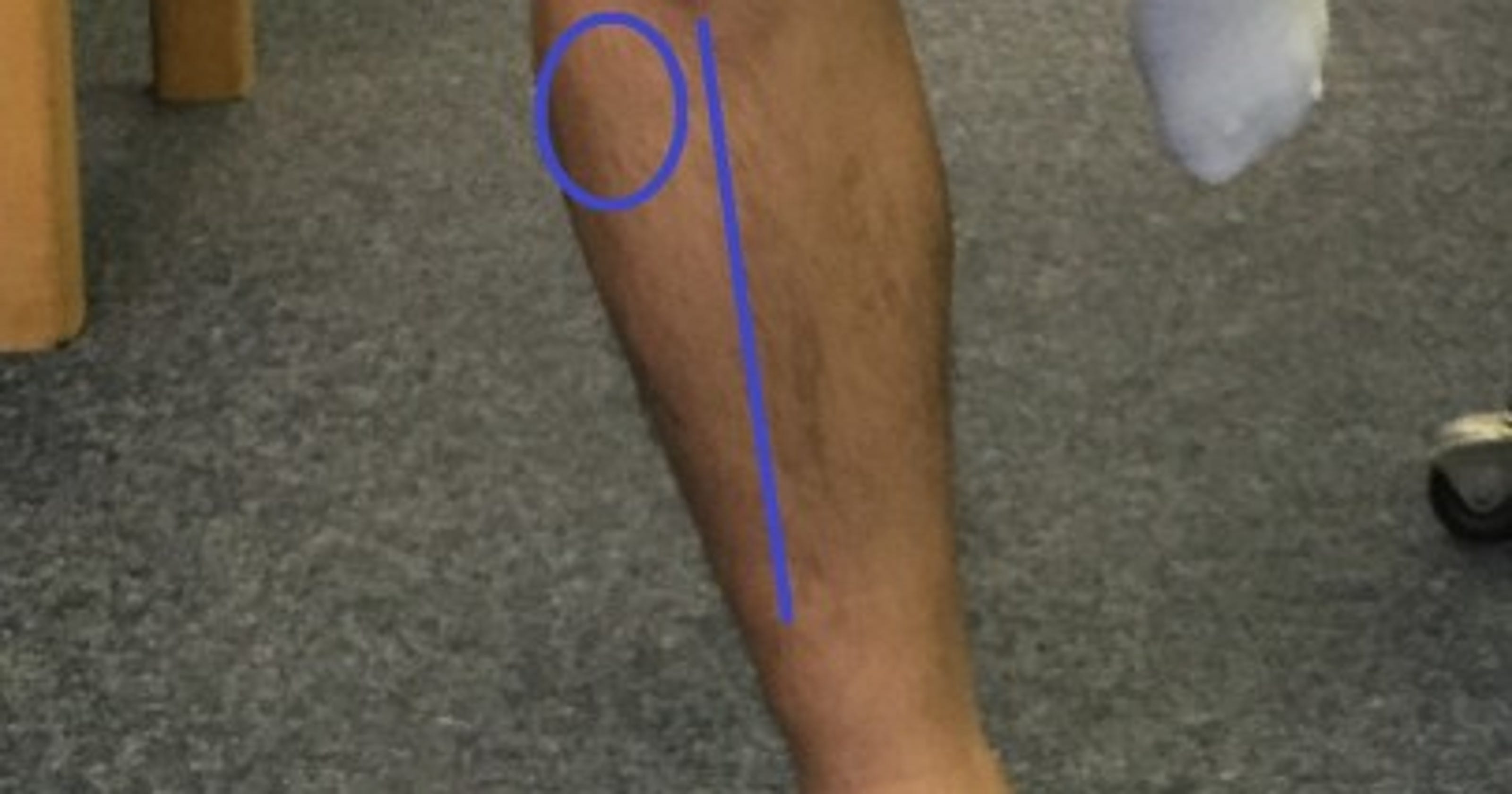
To begin the process of self-assessment and understand how to know if you have shin splints, start by gently palpating the inner edge of your tibia, the shin bone. Use your fingers to press along the bone, from just below the knee down towards the ankle. If you experience tenderness, or a sharp pain when touching a specific area of the bone, it could be an indicator of shin splints. The pain associated with shin splints is usually found along the middle to lower third of the tibia. This technique will help you to focus on the area of concern, and understanding how to know if you have shin splints through self examination. It’s important to note that the pain can vary in intensity and may feel like a dull ache initially that becomes more pronounced when pressure is applied directly to the bone. Be sure to perform this self-examination with gentle pressure, do not apply hard pressure as it can cause pain and further injure the area. This assessment should be done in a relaxed, non-exercise state, preferably after a period of rest. Observing how your body responds to this self palpation can offer important clues to how to know if you have shin splints, in conjunction with other symptoms.
Another practical step in self-assessment involves paying close attention to the nature and location of the pain. To assess how to know if you have shin splints, note if the discomfort is predominantly along the inner edge of the shin bone rather than a more localized spot, which might indicate a different issue. Pain from shin splints is usually more diffuse across a larger area of the shin. A dull ache that gets worse during physical activity, or after exercise, is characteristic of shin splints. To further evaluate how to know if you have shin splints, try some basic movements that would load the shin, such as light hopping or tiptoe standing; if pain increases with these actions, it suggests that the symptoms are more likely related to shin splints. Furthermore, be aware that this self-assessment is an initial step, and it is not a definitive medical diagnosis. This assessment is designed to help you gain more awareness of your body and help with understanding how to know if you have shin splints and should be considered a preliminary step in understanding your symptoms. If your pain continues or if it worsens after self assessment, a consultation with a healthcare professional for a proper diagnosis is recommended.
Understanding The Underlying Causes of Shin Splints
The development of Medial Tibial Stress Syndrome, commonly known as shin splints, is often multifactorial, arising from a combination of physical activities and individual predispositions. Overtraining stands out as a significant contributor; when the muscles and bones of the lower leg are subjected to repetitive stress without adequate rest, they become vulnerable to inflammation and micro-tears. This is particularly true when there’s a rapid increase in training intensity or duration. Another important factor to consider is the choice of footwear. Shoes that lack proper support or cushioning can fail to absorb the impact of each step, transferring more force to the tibia and surrounding tissues. Similarly, engaging in activities on hard or uneven surfaces can heighten the risk. These external elements are not the only causes to be considered when evaluating how to know if you have shin splints; biomechanical issues such as overpronation, where the foot rolls inward excessively upon impact, or flat feet, can alter the normal distribution of force, leading to increased stress on the tibia. Inappropriate techniques while exercising and inadequate stretching of the calf muscles can also exacerbate these issues.
Furthermore, sudden increases in activity levels, such as those seen when beginning a new exercise routine or returning to sports after a period of inactivity, can place excessive demands on the lower legs. These sudden changes often don’t allow the body sufficient time to adapt. The muscles, tendons, and bones are not prepared to handle the new stress and thus become more susceptible to injury, including shin splints. This vulnerability highlights the importance of a progressive training approach to manage how to know if you have shin splints. In addition, it’s important to note that individual factors can also play a role. For example, people with lower bone density, muscle imbalances, or previous injuries in the lower leg may be at increased risk of developing shin splints. Understanding these contributing factors is vital in managing and preventing the condition. When considering how to know if you have shin splints, examining your training routine, footwear, and biomechanics might help you discover the underlying causes of your pain.
Differentiating Shin Splints From Other Lower Leg Conditions
It’s crucial to understand that shin splints, or Medial Tibial Stress Syndrome (MTSS), can sometimes be confused with other lower leg conditions, making it important to know how to know if you have shin splints and differentiate it from other ailments. One common misdiagnosis is stress fractures, which, unlike the more diffuse pain of shin splints, typically present with a very localized, sharp pain at a specific point on the bone. This pain is often more severe, especially at night, and is usually exacerbated by weight-bearing activities. Another condition, compartment syndrome, is characterized by pain, tightness, and sometimes numbness or tingling in the affected leg compartment, most common after physical activity. This condition, unlike shin splints, is associated with a noticeable swelling and tightness in the muscles, and usually the pain will increase during activity and subside at rest but can take hours to resolve. Lastly, tendonitis, which involves inflammation of the tendons, can also mimic shin splint pain. The pain in tendonitis is generally localized to the tendon insertion site, such as the Achilles tendon at the heel or the tibialis anterior tendon along the shin, and is typically aggravated by specific movements associated with the affected tendon. While shin splints cause pain along the inner edge of the tibia, these other conditions usually have specific pain points, it’s important to note that if you are wondering how to know if you have shin splints, a detailed self-assessment can only be the starting point for the final diagnosis.
Understanding the nuanced differences in pain characteristics is vital in the process of self-diagnosis, especially to know how to know if you have shin splints. With stress fractures, the pain is sharply defined and pinpointed, whereas shin splint pain tends to spread across a wider area of the shin bone. Compartment syndrome will also present with signs not found with shin splints, such as tightness, swelling and, in some cases, nerve-related symptoms like numbness. In contrast, tendonitis has a localized pain, often at the joint or tendon area, and could include a burning or stabbing sensation. Differentiating each is very important to accurately assess your condition. If you are trying to understand how to know if you have shin splints, remember that the nature of your pain provides crucial clues; it’s important to pay close attention to whether the pain is a dull ache along the bone, sharp and localized, or associated with swelling and tightness in the muscle compartment, these are key pieces to understanding your condition and the necessary steps you should take.
When to Seek Professional Evaluation for Shin Pain
While self-assessment can offer insights into whether you might have shin splints, it is crucial to recognize when symptoms warrant professional medical attention. Persistent or worsening shin pain should not be ignored, as it could indicate a more serious underlying issue. If your pain intensifies, despite implementing home care strategies such as rest and ice, it’s time to consult a healthcare provider. How to know if you have shin splints sometimes requires ruling out other conditions, and a medical professional can provide a definitive diagnosis, ensuring that appropriate treatment is initiated. Specifically, seek professional evaluation if you experience intense pain that significantly restricts daily activities, especially if the pain is present even when not exercising or is impacting your ability to bear weight comfortably. These are not typical shin splint symptoms, and they might indicate a different issue, such as a stress fracture, which will need medical intervention.
Swelling, redness, or visible deformity of the lower leg also necessitates immediate medical attention. These symptoms could be indicative of inflammation, infection, or a more serious injury that requires prompt treatment. Moreover, if pain persists for more than a couple of weeks despite initial home management, it is advisable to seek a consultation with a healthcare professional. Relying solely on self-treatment in cases of prolonged or worsening symptoms may delay proper care and potentially exacerbate the condition. Remember, while understanding how to know if you have shin splints through self-assessment is a valuable skill, it is not a substitute for a comprehensive medical examination by a qualified practitioner, who will provide a precise diagnosis and an appropriate treatment plan. Early consultation allows for a more effective management of symptoms, and an earlier return to activity. For a correct diagnosis, an assessment with a professional will be required.
Home Care and Initial Management Strategies for Shin Splint Symptoms
When experiencing shin pain, initial home care strategies can provide relief and help manage symptoms. Rest is paramount; this means reducing or ceasing activities that aggravate the pain. Avoid high-impact exercises like running or jumping, and give your legs the chance to recover. The application of ice is another key component of managing symptoms. Wrap ice in a thin cloth and apply to the affected area for 15 to 20 minutes at a time, several times a day. This helps reduce inflammation and pain. Over-the-counter pain relievers, such as ibuprofen or naproxen, can also provide temporary relief by reducing inflammation and discomfort. It’s essential to adhere to the recommended dosage and consult a healthcare professional if you have underlying health conditions or are taking other medications. These initial steps are not a replacement for professional medical advice, but they offer a first line of defense after a self-assessment of your symptoms and if you are wondering how to know if you have shin splints, these methods can help reduce the discomfort.
To support the healing process, consider using supportive footwear, even during periods of rest. Avoid flat or unsupportive shoes and instead use something with good arch support and cushioning. Gentle stretching of the calf muscles and surrounding tissues may also help alleviate some pain, but should be done with caution and only if it doesn’t exacerbate the symptoms. Focus on stretches that don’t cause additional pain. The best approach is to take some time off from the aggravating activity and give the muscles time to heal. Remember that these are initial management strategies and not a long-term solution. If the pain persists or worsens despite these efforts, or if you are still unclear how to know if you have shin splints, seeking professional evaluation is necessary for proper diagnosis and treatment. This initial management strategy can provide valuable relief while you are waiting for your appointment with a medical professional and helps with the management of pain and symptoms. Being proactive with home care will help you start the recovery journey.
Preventing Shin Splint Recurrence
Preventing the recurrence of shin splints, also known as Medial Tibial Stress Syndrome (MTSS), is crucial for maintaining consistent physical activity and overall lower leg health. A proactive approach that combines smart training practices with attentive self-care can dramatically reduce the risk of experiencing this painful condition again. A cornerstone of prevention is understanding and adhering to proper training progression. Abrupt increases in training intensity or duration are significant contributors to shin splints. It is essential to gradually increase the load on the lower legs to allow the muscles, tendons, and bones to adapt. This means not increasing weekly mileage or the intensity of workouts by more than 10% at a time, for running activities for example, this is especially important in understanding how to know if you have shin splints in its early stages, as pain will be minimal but consistent. Another key preventative measure is the selection and use of appropriate footwear. Running shoes, in particular, should be fitted to the individual’s foot type and activity, and should be replaced regularly to ensure they still offer adequate cushioning and support. Worn-out shoes can contribute to increased stress on the lower legs. Incorporating a regimen of regular stretching and strengthening exercises is also vital for long-term shin splint prevention. Specific stretches for the calf muscles, such as soleus and gastrocnemius stretches, can help improve flexibility, which reduces stress on the tibia. Strengthening exercises such as calf raises, toe raises, and tibialis anterior raises can also improve muscle support, stability, and shock absorption.
In addition to these proactive steps, it’s essential to pay close attention to the body’s signals of fatigue or discomfort, particularly understanding how to know if you have shin splints. Ignoring these warnings can lead to recurring shin splint episodes. Rest and recovery are just as important as training, so ensuring there are adequate rest days can also support prevention. If you have experienced shin splints before, understanding the need to prevent them is crucial, consider modifying your training routine with low-impact cross-training activities, such as swimming or cycling, when possible to allow the lower legs to recover. These activities will keep fitness levels up while reducing the risk of recurrence. Moreover, you must be aware of your running surface, and avoid uneven and hard terrains as much as possible. Addressing biomechanical issues, such as overpronation or supination, may also be necessary. This may require the use of custom orthotics or consulting with a physical therapist to develop an individualized plan. By integrating all these preventative measures, it is feasible to substantially reduce the likelihood of experiencing shin splints, allowing individuals to enjoy physical activities with less discomfort. By recognizing the significance of these preventive strategies, long-term physical health can be achieved.