Recognizing the Symptoms of a Collapsed Lung
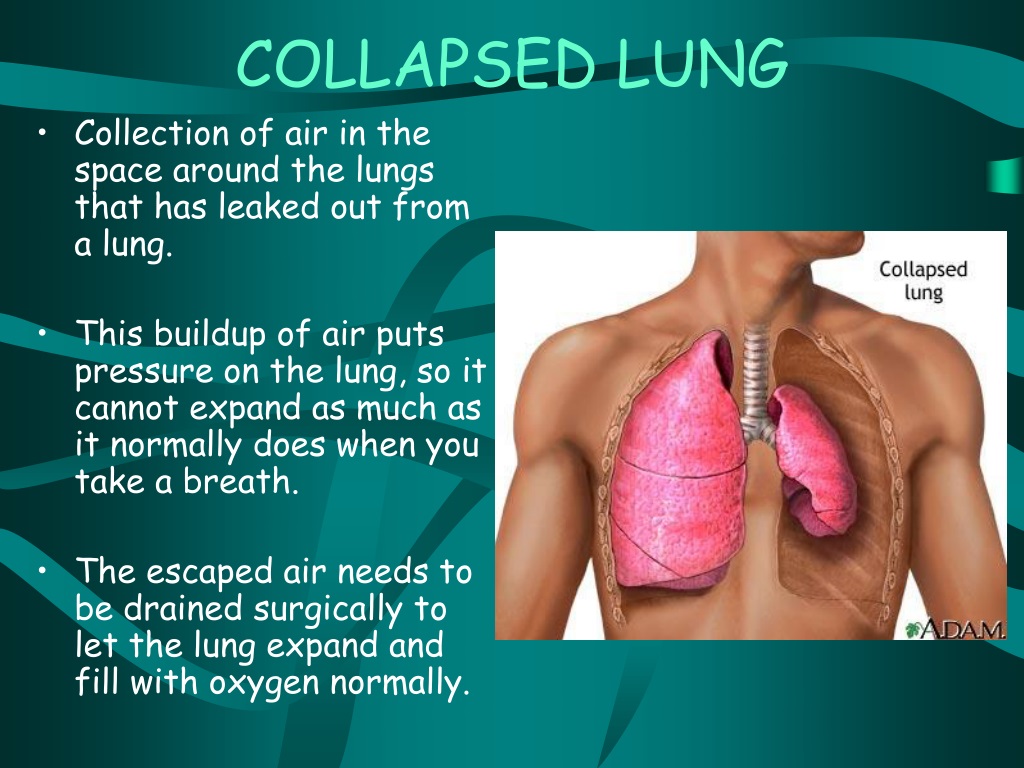
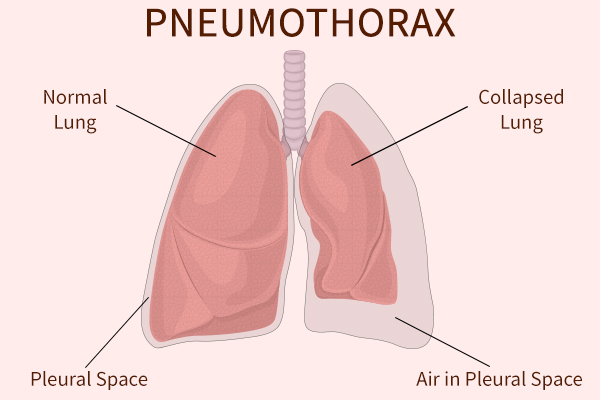
A collapsed lung, also known as pneumothorax, can be a life-threatening condition if not treated promptly. It occurs when air leaks into the space between the lung and the chest wall, causing the lung to collapse partially or completely. Understanding the symptoms of a collapsed lung is crucial for seeking immediate medical attention. Common signs and symptoms include:
- Chest pain: Sudden, sharp, or stabbing pain in the chest, usually on one side, which may worsen when breathing deeply, coughing, or changing positions.
- Shortness of breath: Difficulty breathing or feeling like you can’t get enough air, which may be more pronounced when engaging in physical activities.
- Rapid heartbeat: Increased pulse rate, often accompanied by feelings of anxiety or restlessness.
- Fatigue: Unexplained tiredness or weakness, which may be more pronounced if you have an underlying medical condition.
- Bluish skin: Discoloration of the lips, fingertips, or face, indicating a lack of oxygen in the blood.
- Cough: Persistent cough, which may produce clear, blood-tinged, or frothy sputum.
- Wheezing: Whistling or rasping sounds when breathing, which may indicate partial airway obstruction.
- Dizziness or fainting: Lightheadedness, confusion, or loss of consciousness, which may occur due to insufficient oxygen supply to the brain.
If you suspect a collapsed lung or experience any of these symptoms, it is essential to consult a healthcare professional immediately. Delaying medical treatment can lead to severe complications, such as respiratory failure or even death. Early diagnosis and appropriate intervention can significantly improve the prognosis and minimize the risk of long-term lung damage.
Understanding the Causes of a Collapsed Lung
A collapsed lung, or pneumothorax, can be caused by various factors, which can be broadly categorized into injuries, underlying medical conditions, and lifestyle factors. Understanding these causes can help individuals take preventive measures and seek prompt medical attention when necessary.
Injuries
Physical trauma to the chest, such as blunt force or penetrating injuries, can result in a collapsed lung. Common causes of injury-related pneumothorax include:
- Motor vehicle accidents
- Sports-related injuries
- Falls or blows to the chest
- Rib fractures
- Stab or gunshot wounds
Underlying Medical Conditions
Certain medical conditions can increase the risk of a collapsed lung. These conditions include:
- Chronic Obstructive Pulmonary Disease (COPD): This progressive lung disease, which includes emphysema and chronic bronchitis, can weaken lung tissue and make it more susceptible to collapse.
- Asthma: Severe asthma attacks can cause the airways to narrow and become overinflated, leading to a collapsed lung.
- Cystic fibrosis: This genetic disorder affects the mucus-producing glands, leading to thick, sticky mucus that can clog the airways and cause a collapsed lung.
- Tuberculosis (TB): This infectious disease can cause lung tissue to scar and become fragile, increasing the risk of a collapsed lung.
- Pneumonia: Severe cases of pneumonia can cause lung tissue to become inflamed and weakened, making it more susceptible to collapse.
Lifestyle Factors
Certain lifestyle choices can also contribute to the development of a collapsed lung, such as:
- Smoking: Smoking damages the lung tissue, making it more prone to collapse. Additionally, smokers are more likely to develop COPD, which further increases the risk.
- Scuba diving: Rapid changes in pressure during scuba diving can cause lung overexpansion and lead to a collapsed lung, especially in individuals with pre-existing lung conditions.
- Illegal drug use: Inhaling drugs, such as crack cocaine, can damage the lung tissue and increase the risk of a collapsed lung.
By understanding the causes of a collapsed lung, individuals can take proactive steps to reduce their risk and seek timely medical attention if symptoms arise. Early diagnosis and appropriate treatment can significantly improve the prognosis and minimize the risk of long-term lung damage.
Immediate Medical Attention: When to Consult a Healthcare Professional
A collapsed lung, or pneumothorax, is a medical emergency that requires prompt attention from a healthcare professional. Delaying treatment can lead to severe complications, such as respiratory failure, cardiac arrest, or even death. If you suspect a collapsed lung or experience related symptoms, seek medical help immediately.
The following situations warrant consulting a healthcare professional:
- Sudden, sharp, or stabbing chest pain, especially when accompanied by shortness of breath, rapid heartbeat, or dizziness.
- A history of trauma or injury to the chest, even if no symptoms are present.
- Recent scuba diving or high-altitude activities, especially if you have a history of lung conditions or respiratory issues.
- A known diagnosis of an underlying medical condition that increases the risk of a collapsed lung, such as COPD, asthma, or cystic fibrosis.
- Persistent cough, wheezing, or difficulty breathing, even if these symptoms are mild or intermittent.
- Unexplained fatigue, bluish skin, or fainting, which may indicate a lack of oxygen in the blood.
Healthcare professionals will assess your symptoms, medical history, and risk factors to determine whether a collapsed lung is likely. They may order diagnostic tests, such as chest X-rays, CT scans, or blood tests, to confirm the diagnosis and evaluate the extent of the damage. Based on the test results, they will develop an appropriate treatment plan to repair the collapsed lung and prevent future occurrences.
Remember, when it comes to a collapsed lung, time is of the essence. Seeking immediate medical attention can significantly improve the prognosis and minimize the risk of long-term lung damage. By being aware of the symptoms and risk factors, you can take proactive steps to protect your lung health and ensure prompt treatment if necessary.
Diagnostic Procedures: How Doctors Identify a Collapsed Lung
Healthcare professionals use various diagnostic tests and procedures to confirm a collapsed lung, determine the extent of the damage, and develop an appropriate treatment plan. These tests may include:
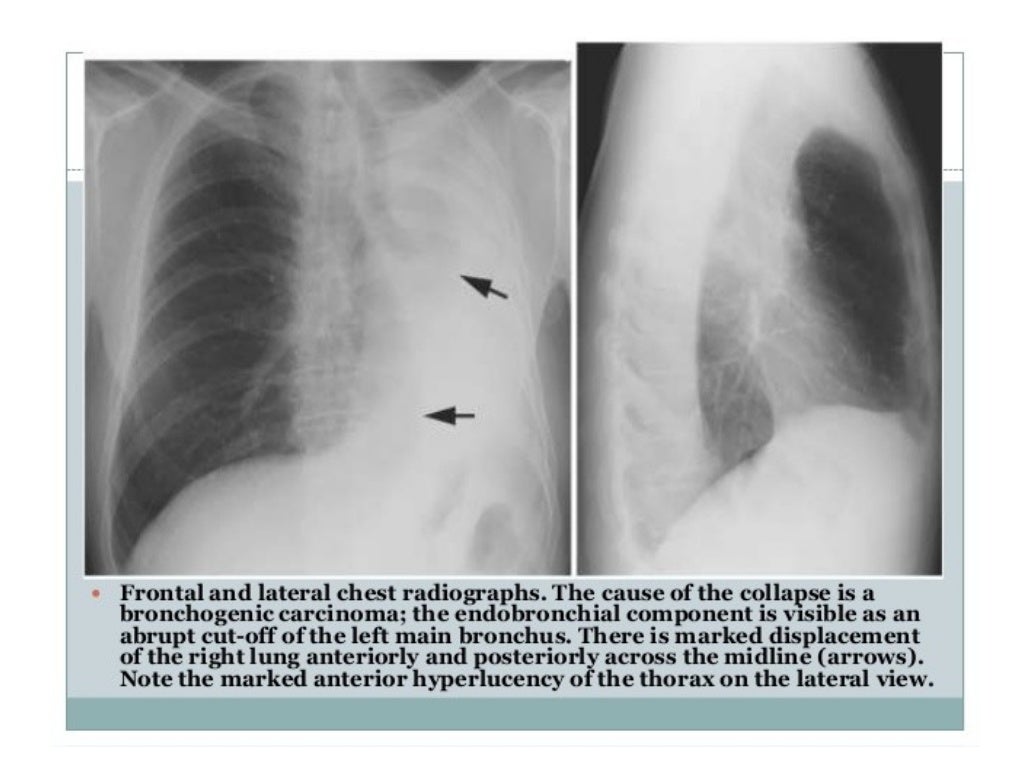
Chest X-ray
A chest X-ray is often the first diagnostic test performed when a collapsed lung is suspected. It uses a small amount of radiation to create images of the structures inside the chest, including the lungs, heart, and blood vessels. A chest X-ray can reveal air outside the lung tissue, which indicates a collapsed lung.
Computed Tomography (CT) Scan
A CT scan combines multiple X-ray images taken from different angles to create detailed cross-sectional images of the chest. This test can provide more information about the size, location, and severity of the collapsed lung, as well as any underlying conditions contributing to the collapse. CT scans use more radiation than chest X-rays, but they can be essential for developing a comprehensive treatment plan.
Blood Tests
Blood tests can help healthcare professionals assess the overall health of the patient, identify any underlying medical conditions, and evaluate the body’s response to the collapsed lung. Blood tests may include:
- Arterial blood gas (ABG) analysis: Measures the oxygen and carbon dioxide levels in the blood to assess lung function and oxygenation.
- Complete blood count (CBC): Evaluates the number and type of blood cells, which can help identify infections, anemia, or other conditions.
- Electrolyte panel: Assesses the balance of essential minerals, such as sodium, potassium, and chloride, which can be affected by lung conditions or treatments.
Ultrasound
An ultrasound uses high-frequency sound waves to create real-time images of the internal organs. While not as commonly used as chest X-rays or CT scans, ultrasounds can be helpful in certain situations, such as identifying a collapsed lung in pregnant women or patients with contraindications for radiation exposure.
Additional Diagnostic Tests
Depending on the patient’s symptoms and medical history, healthcare professionals may also order additional tests, such as:
- Pulmonary function tests (PFTs): Measures the lung’s ability to exchange oxygen and carbon dioxide effectively.
- Echocardiogram: Uses ultrasound to evaluate the heart’s structure and function, which can be affected by a collapsed lung or underlying medical conditions.
- Magnetic resonance imaging (MRI): Uses magnetic fields and radio waves to create detailed images of the body’s internal structures, which can be helpful in identifying underlying conditions or complications related to a collapsed lung.
By utilizing these diagnostic procedures, healthcare professionals can accurately diagnose a collapsed lung, determine the best course of treatment, and monitor the patient’s progress throughout the recovery process.
Treatment Options: Repairing a Collapsed Lung
Treatment for a collapsed lung, or pneumothorax, depends on the severity of the collapse, the underlying cause, and the patient’s overall health. Healthcare professionals typically consider the following treatment options:
Oxygen Therapy
Oxygen therapy involves administering supplemental oxygen through a nasal cannula or face mask. This treatment helps ensure the body receives adequate oxygen while the lung heals. Oxygen therapy may be sufficient for minor collapses or as a supportive measure during more invasive treatments.
Chest Tube Insertion
For more severe collapses, healthcare professionals may insert a chest tube to remove the excess air or fluid accumulated between the lung and the chest wall. The tube is typically connected to a vacuum device that applies continuous suction, allowing the lung to re-expand gradually. Chest tube insertion is usually performed under local anesthesia and may require hospitalization for monitoring and management.
Surgical Intervention
Surgery may be necessary for recurrent or persistent collapsed lungs, large or tension pneumothoraces, or cases where other treatments have been unsuccessful. Surgical options include:
- Video-assisted thoracoscopic surgery (VATS): A minimally invasive procedure that uses a small camera and specialized instruments to access the chest cavity. Surgeons can repair damaged lung tissue, seal air leaks, and remove any accumulated fluid or blood.
- Thoracotomy: An open surgical procedure that involves making a larger incision in the chest to access the affected lung. This approach is typically reserved for complex cases or when VATS is not feasible. Thoracotomy allows for more extensive repairs and may be combined with a lobectomy (removal of a lung lobe) if necessary.
Benefits and Risks
Each treatment option carries its own benefits and risks. Oxygen therapy is generally safe and non-invasive but may not be sufficient for severe collapses. Chest tube insertion effectively removes excess air or fluid but can be painful and may lead to complications, such as infection, bleeding, or injury to surrounding structures.
Surgical intervention can provide definitive treatment for recurrent or persistent collapsed lungs but carries the risks associated with anesthesia, infection, and potential lung damage. It is essential to discuss the benefits and risks of each treatment option with a healthcare professional to determine the most appropriate course of action for individual circumstances.
In some cases, healthcare professionals may recommend preventive measures, such as pleurodesis (sealing the lung lining to prevent future collapses) or surgical pleurectomy (removal of the lung lining), to reduce the risk of recurrence. These procedures are typically considered after a patient has experienced multiple collapsed lungs.
Post-Treatment Recovery: What to Expect After Repairing a Collapsed Lung
Recovery from a collapsed lung, or pneumothorax, can vary depending on the severity of the collapse, the underlying cause, and the treatment received. In general, patients can expect the following recovery process:
Hospitalization and Monitoring
After treatment, patients may need to stay in the hospital for observation and monitoring. The duration of hospitalization can range from a few days to over a week, depending on the individual’s progress and overall health. During this time, healthcare professionals will assess lung function, manage pain, and address any complications that may arise.
Lifestyle Changes
To promote optimal healing and reduce the risk of recurrence, patients may need to make certain lifestyle changes, such as:
- Quitting smoking: Smoking damages the lungs and increases the risk of collapsed lungs. Patients who smoke should consult their healthcare team for resources and support to quit.
- Avoiding strenuous activities: Patients should avoid heavy lifting, contact sports, or other activities that may put strain on the lungs during the recovery period. Gradually reintroducing physical activities under the guidance of a healthcare professional is essential.
- Maintaining a healthy diet: A balanced diet rich in fruits, vegetables, lean proteins, and whole grains can support lung health and overall recovery.
- Staying hydrated: Drinking plenty of water can help thin mucus and maintain lung function.
Follow-up Appointments
Regular follow-up appointments with a healthcare professional are crucial to monitor recovery progress, address any concerns, and identify potential complications early. Patients should schedule and attend all recommended appointments and discuss any changes in symptoms or concerns with their healthcare team.
Potential Restrictions
Depending on the severity of the collapsed lung and the treatment received, patients may need to adhere to certain restrictions, such as avoiding air travel, scuba diving, or high-altitude activities until cleared by a healthcare professional. These restrictions help minimize the risk of lung barotrauma and recurrence.
Open Communication
Maintaining open communication with the healthcare team throughout the recovery process is essential. Patients should feel comfortable discussing their progress, concerns, and any new symptoms with their healthcare professionals. This collaboration ensures the best possible outcomes and supports long-term lung health.
By understanding the recovery process and following the recommended guidelines, patients can successfully heal from a collapsed lung and reduce the risk of future collapses. Staying proactive, informed, and engaged in their healthcare is crucial for managing lung health and maintaining an optimal quality of life.
Preventing Future Collapsed Lungs: Tips and Recommendations
Taking preventive measures to reduce the risk of experiencing another collapsed lung is crucial for maintaining long-term lung health. Consider the following tips and recommendations:
Avoid Smoking
Smoking damages the lungs and increases the risk of collapsed lungs. Quitting smoking is one of the most effective ways to reduce the likelihood of future collapses. Patients should consult their healthcare team for resources and support to quit smoking.
Practice Safe Physical Activities
Participating in high-impact or contact sports can increase the risk of lung injury and collapse. Patients should consider low-impact activities, such as swimming, cycling, or yoga, and always use proper protective gear when engaging in potentially hazardous activities.
Maintain a Healthy Lifestyle
Eating a balanced diet, exercising regularly, and getting adequate sleep can help strengthen the lungs and improve overall health. A healthy lifestyle can also reduce the risk of developing underlying medical conditions that may contribute to collapsed lungs.
Address Respiratory Issues Promptly
Persistent cough, chest pain, or shortness of breath should be evaluated by a healthcare professional as soon as possible. Early intervention can help prevent lung damage and potential collapses.
Regular Check-ups
Regular check-ups with a healthcare professional can help identify any underlying conditions or risk factors that may increase the likelihood of a collapsed lung. Early detection and management can significantly reduce the risk of future collapses.
Seek Medical Attention for Chest Injuries
Chest injuries, no matter how minor, should be evaluated by a healthcare professional. Prompt medical attention can help prevent lung damage and potential collapses.
Consider Pleurodesis or Pleurectomy
For patients with a history of recurrent collapsed lungs, healthcare professionals may recommend pleurodesis or pleurectomy. These procedures involve sealing the lung lining or removing the lung lining to prevent future collapses. Discuss the benefits and risks of these procedures with a healthcare professional to determine if they are appropriate.
By following these tips and recommendations, patients can significantly reduce their risk of experiencing another collapsed lung and maintain optimal lung health. Staying proactive, informed, and engaged in their healthcare is essential for managing lung health and maintaining an optimal quality of life.
Living with a History of Collapsed Lungs: Stories of Resilience
A collapsed lung, or pneumothorax, can be a frightening experience, but many individuals have successfully recovered and resumed their normal activities. Here are a few inspiring stories of resilience:
John’s Story: From Athlete to Advocate
John, a college athlete, experienced a collapsed lung during a high-impact workout. After undergoing treatment and making a full recovery, John became an advocate for lung health, sharing his story to raise awareness about the importance of proper exercise techniques and protective gear. Today, John is back to competing in his favorite sports and encourages others to prioritize their lung health.
Sarah’s Story: Overcoming Chronic Conditions
Sarah, a mother of two, struggled with chronic respiratory issues that led to multiple collapsed lungs. Despite the challenges, Sarah remained determined to regain her lung health. Through a combination of medical treatments, lifestyle changes, and perseverance, Sarah successfully recovered and now enjoys an active, fulfilling life with her family.
Michael’s Story: A Second Chance at Life
Michael, a construction worker, suffered a severe chest injury that resulted in a collapsed lung. The experience served as a wake-up call for Michael, who had previously neglected his lung health. After making significant lifestyle changes, including quitting smoking and adopting a healthier diet, Michael successfully recovered and returned to work with renewed vigor and appreciation for life.
These stories of resilience demonstrate that, even after a collapsed lung, individuals can recover and resume their normal activities. By remaining hopeful, proactive, and committed to managing their lung health, patients can overcome the challenges associated with a collapsed lung and enjoy a fulfilling life.