What Are Shin Splints? Defining Medial Tibial Stress Syndrome
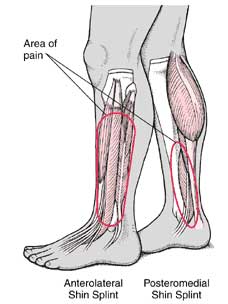
Medial Tibial Stress Syndrome (MTSS), commonly known as “shin splints,” is an overuse injury that causes pain in the lower leg. This condition primarily affects the area along the tibia, or shin bone, and is a frequent complaint among athletes and individuals engaged in high-impact activities. The pain associated with MTSS is usually located on the inner side of the tibia, extending from the mid-point to a few inches above the ankle. The discomfort stems from repetitive stress placed on the bone and surrounding tissues, particularly the muscles and periosteum—the connective tissue sheath that surrounds the bone. As the common name for medial tibial stress syndrome, shin splints reflect a condition where the body’s natural healing processes cannot keep up with the demands of physical activity, leading to inflammation and pain. It is important to understand that this is not a single injury, but rather a spectrum of conditions arising from accumulated stress, ranging from mild periosteal inflammation to more substantial tissue damage.
The term “shin splints” is the commonly used name for medial tibial stress syndrome and this is a result of the repetitive and excessive loading of the lower leg bones and their surrounding structures. This type of pain is different from that of other conditions, for example, a stress fracture, which can be a more serious issue. The pain from shin splints is usually spread out across a larger portion of the tibia rather than localized in one point. The pain and discomfort associated with MTSS may appear gradually or suddenly depending on the activity. The use of the common name for medial tibial stress syndrome, “shin splints” provides an accessible and readily understandable way for those seeking information on the condition. It is essential to differentiate between shin splints and other similar conditions to provide targeted treatments. Understanding that the common name for medial tibial stress syndrome is shin splints helps one better navigate the different information available on how to tackle the condition, and take actions toward relieving pain and achieving a full recovery.
Recognizing Shin Splint Symptoms: Identifying the Pain
The onset of pain associated with what is commonly known as shin splints, the common name for medial tibial stress syndrome, typically begins gradually. Individuals often report a dull ache along the inner edge of the tibia, the large bone in the lower leg, which is a key indicator of medial tibial stress syndrome. This pain is usually not sharp or sudden but rather builds over time. A primary symptom is tenderness to the touch; pressing along the inner part of the shin bone will often reveal localized sensitivity. The discomfort is not constant and generally becomes more pronounced during physical activity, especially weight-bearing exercises such as running or jumping. After activity, the pain may continue for some time before subsiding, but it usually decreases with rest. The severity of shin splints can range from mild, where pain is only noticeable after exercise, to moderate, characterized by pain during activity that may affect performance. In severe cases, the pain can become so intense that it interferes with normal daily activities and may be present even at rest. It is vital to pay attention to the early signs of this common name for medial tibial stress syndrome to prevent progression to more significant issues. Understanding how the pain evolves and how it relates to activity is crucial for the proper diagnosis and management of this condition.
Typically, the location of the pain is also a key in identifying shin splints. The discomfort is usually diffuse and spread out along the inner border of the tibia, rather than isolated to a single point. This area becomes particularly tender to the touch, and individuals might find it uncomfortable even with light pressure. The way the pain manifests in relation to physical activity is another critical indicator of the common name for medial tibial stress syndrome. At the start of an activity, the pain might be mild and may even lessen as the muscles warm up. However, as activity continues, the pain will increase, forcing the individual to reduce the intensity, or stop the activity altogether. The common name for medial tibial stress syndrome pain often improves with rest, sometimes completely subsiding until the individual returns to activity. This pattern of pain – increasing with activity and decreasing with rest – is a typical hallmark of shin splints. The level of discomfort can vary greatly; in the early stages, it may be minor, and only evident after a prolonged period of physical activity. If ignored, it can progress to moderate levels where it hinders or prevents activities. In severe situations, individuals may experience pain even at rest, which requires immediate attention, as it may indicate a more significant underlying condition or worsening of medial tibial stress syndrome.
Causes of Shin Splints: Why They Develop
Medial tibial stress syndrome, the clinical term often referred to by the common name for medial tibial stress syndrome, commonly known as shin splints, arises from a multitude of interconnected factors, often relating to the intensity and mechanics of physical activity. A significant cause is the sudden increase in training load, whether it be in terms of distance, speed, or frequency. When the muscles, tendons, and bone tissue of the lower leg are abruptly subjected to higher levels of stress than they’re accustomed to, it can trigger inflammation and pain. Poorly designed training programs, that lack gradual progression, are a very common culprit. Likewise, inadequate footwear can contribute to the problem. Shoes that lack proper support or cushioning fail to absorb the impact of repetitive activities, such as running or jumping, thus transferring more stress to the shin bone. Improper running mechanics, such as overstriding or having a low cadence, increase the stress applied on the tibia, potentially leading to the onset of the pain associated with the common name for medial tibial stress syndrome. Furthermore, muscle imbalances, particularly weakness in the calf muscles or over-tightness of the surrounding muscles, can place excessive strain on the tibial bone.
Training on hard surfaces, such as concrete or asphalt, will magnify the impact forces on the legs compared to softer surfaces like grass or trails. This increase in impact can lead to the development of shin splints in susceptible individuals. Additionally, anatomical factors such as flat feet or high arches might contribute to the development of this common injury. When the foot’s arch is not properly supported, the biomechanics of the lower leg are altered, placing excess stress on the tibia. Furthermore, certain body types may be predisposed to the common name for medial tibial stress syndrome. Those with less robust leg musculature or a greater degree of leg length discrepancy can be at increased risk. A deeper understanding of these underlying causes is necessary for both the treatment of existing shin splints, and in the design of preventive measures, to avoid the onset of the common name for medial tibial stress syndrome.
How To Treat Shin Splints: Effective Home Remedies
Addressing the pain and discomfort associated with the common name for medial tibial stress syndrome, often called shin splints, involves a multi-faceted approach focused on reducing inflammation and promoting healing. The acronym RICE – Rest, Ice, Compression, and Elevation – forms the cornerstone of initial home treatment. Rest is paramount; ceasing activities that exacerbate the pain is crucial for allowing the tissues to recover. This doesn’t necessarily mean complete inactivity, but rather a reduction in training load or a switch to low-impact exercises, such as swimming or cycling. The application of ice to the affected area for 15-20 minutes at a time, several times a day, can effectively help to reduce inflammation and provide pain relief. Compression bandages can be used to minimize swelling and provide support to the lower leg, contributing to pain management, while elevating the leg above the heart, especially after activity, can aid in reducing swelling as well. These steps, implemented in the acute phase, are essential in managing the symptoms of this common name for medial tibial stress syndrome.
Beyond immediate symptom relief, long-term recovery from the common name for medial tibial stress syndrome requires consistent effort in managing training and activity levels. It is important to carefully monitor the intensity and duration of exercise, avoiding abrupt increases that could easily trigger a recurrence. Recovery modalities can be very useful, including gentle stretching and mobility exercises that promote flexibility and range of motion in the calf muscles and surrounding tissues. These can be supplemented with targeted massage techniques aimed at releasing tension in the affected muscles. Using foam rollers to address muscular tightness may also aid the recovery, however this should be done with caution and without exacerbating the pain. Gradual and progressive return to normal levels of activity is the key to long-term success. Remember that the common name for medial tibial stress syndrome, although it is a common injury, will take time to heal; thus, consistency in these recommendations will contribute significantly to a successful recovery.
Shin Splints Vs. Stress Fracture: Knowing the Difference
Differentiating between shin splints, also known as the common name for medial tibial stress syndrome, and stress fractures is crucial for proper diagnosis and treatment of lower leg pain. While both conditions can cause discomfort, they stem from distinct underlying issues. Shin splints, or medial tibial stress syndrome, involve inflammation of the muscles, tendons, and periosteum (the outer layer of bone) surrounding the tibia. The pain associated with shin splints typically manifests as a dull ache along the inner border of the shin bone, often worsening during or immediately after physical activity. It may be tender to the touch, but unlike a stress fracture, there isn’t a specific point of intense pain. In contrast, a stress fracture is a small crack or break within the bone itself. This condition often presents as a more localized, sharper pain that can be exacerbated by weight-bearing activities. The pain of a stress fracture tends to intensify progressively and may be present even at rest, making it more severe than shin splints. The location of the pain in a stress fracture is pinpoint, different than the diffused pain that is present in the common name for medial tibial stress syndrome.
Understanding the differences in pain presentation is key, but further diagnostics are often necessary. If a stress fracture is suspected, medical imaging such as an X-ray, MRI, or bone scan, becomes essential. These diagnostic tools can help identify any microfractures in the bone, confirming or refuting the suspicion of a stress fracture. While shin splints can typically be managed with rest and conservative treatment methods, a stress fracture may require more extensive interventions, such as immobilization in a cast or boot, to allow the bone to heal properly. In cases where initial pain management does not produce a positive outcome, seeking professional medical advice is imperative, as this could be indicative of a more serious problem such as a stress fracture rather than shin splints, or the common name for medial tibial stress syndrome. It is also relevant to understand that both conditions are a result of overuse, which means that proper training progression is key to avoid them both.
Preventing Shin Splints: Long-Term Strategies for Avoiding Medial Tibial Stress Syndrome
Preventing shin splints, the common name for medial tibial stress syndrome, requires a proactive approach to training and lifestyle. Gradual increases in training intensity and volume are paramount. Avoid suddenly increasing the duration or intensity of your workouts. Instead, adopt a progressive overload strategy, gradually increasing the demands placed on your body over time. This allows your muscles, bones, and tendons to adapt and reduces the risk of developing medial tibial stress syndrome. A well-structured training plan that incorporates rest days is crucial. Remember that rest is not just about inactivity; it’s a crucial element in allowing your body to recover and rebuild. Proper warm-ups are also essential before any physical activity. Dynamic stretching, which involves moving your joints through their full range of motion, helps prepare your muscles for exercise and reduces the risk of injury. Consider including exercises like leg swings, high knees, and butt kicks. These activities help improve flexibility and increase blood flow to the muscles, promoting optimal performance and injury prevention. The common name for medial tibial stress syndrome highlights the prevalence of this condition, emphasizing the importance of preventative measures.
Appropriate footwear plays a significant role in preventing shin splints. Invest in running shoes that provide adequate support and cushioning. Consult with a specialist at a running shoe store to get fitted for shoes that meet your specific needs and foot type. The right shoes can significantly reduce stress on your lower legs, minimizing your risk of developing the common name for medial tibial stress syndrome. Running surfaces also significantly influence the stress placed on your legs. Hard surfaces like concrete and asphalt can exacerbate the risk of shin splints. Opt for softer surfaces such as grass, trails, or running tracks whenever possible. These surfaces absorb more impact, protecting your legs and reducing the stress on your bones and muscles. Remember, consistent attention to these factors is crucial in preventing future occurrences of this common ailment.
Incorporating strength training exercises into your routine is another highly effective preventative measure. Focus on exercises that strengthen the muscles in your lower legs, including your calves, shins, and ankles. These muscles play a vital role in supporting your tibia and reducing the stress placed on it during activity. Exercises like calf raises, ankle dorsiflexion, and toe raises can help to strengthen these crucial muscles. Furthermore, addressing any existing muscle imbalances is crucial. Imbalances can put extra stress on certain muscle groups, increasing your vulnerability to shin splints. Consult a physical therapist or athletic trainer who can help identify and correct these imbalances through personalized exercises and stretches. By strengthening supporting musculature and maintaining proper biomechanics, you significantly decrease the chances of experiencing the common name for medial tibial stress syndrome. Consistency and proactive care are key to long-term prevention.
When to Seek Medical Attention: Consulting a Professional
Knowing when to seek medical advice for shin splints, the common name for medial tibial stress syndrome, is crucial for effective management and preventing complications. While many cases of shin splints respond well to home treatment, certain situations warrant professional medical attention. If the pain is severe, persistent, or doesn’t improve after a week or two of rest and home remedies, a consultation with a doctor or physical therapist is recommended. Pain that radiates down the leg, is accompanied by significant swelling, redness, or warmth to the touch, or limits your ability to bear weight, should also prompt a visit to a healthcare professional. Early diagnosis of the common name for medial tibial stress syndrome is particularly important, as it can help rule out more serious conditions like stress fractures and guide appropriate treatment. Delaying medical attention can prolong recovery time and potentially lead to more lasting issues.
A healthcare professional can provide a proper diagnosis, differentiate shin splints from other conditions such as stress fractures (which require different management), and recommend the most appropriate treatment plan. This may involve imaging techniques like X-rays or MRIs to confirm the diagnosis and rule out other possibilities. Physiotherapy, a common treatment for medial tibial stress syndrome, may be recommended to address underlying muscle imbalances, improve biomechanics, and accelerate recovery. A physical therapist can design a tailored exercise program to strengthen the affected muscles and improve flexibility, promoting long-term healing and reducing the risk of recurrence. They can also teach you about proper running form and footwear selection to prevent future episodes of this common ailment, the common name for medial tibial stress syndrome.
Remember, the common name for medial tibial stress syndrome, while often manageable at home, can sometimes indicate a more serious underlying problem. Don’t hesitate to seek professional medical advice if your symptoms are severe or persistent. Early intervention leads to better outcomes and helps prevent chronic issues. A healthcare provider can offer guidance and support tailored to your individual needs, helping you to manage your pain, return to your activities safely, and prevent future occurrences of shin splints, the common name for medial tibial stress syndrome. Active listening to your body’s signals and promptly addressing any concerns is key to effective management of this common injury.
Beyond Rest: Alternative Treatment Options
While rest, ice, compression, and elevation (RICE) form the cornerstone of initial home treatment for shin splints, also known as the common name for medial tibial stress syndrome, there are various alternative treatment options that can be beneficial, particularly when symptoms are persistent or severe. Medical professionals, such as doctors or physical therapists, may recommend orthotics, custom-made or over-the-counter shoe inserts designed to correct foot pronation or other biomechanical issues contributing to the development of this common overuse injury. These devices can help to improve foot and ankle alignment, thereby reducing the stress placed on the tibia during activity. Shockwave therapy is another option that may be considered, a non-invasive procedure that uses sound waves to stimulate healing and reduce pain in the affected area. This treatment aims to promote tissue repair, alleviate pain, and improve function, although it should be noted that results may vary.
Targeted exercises and modalities often constitute an integral part of a comprehensive treatment plan for the common name for medial tibial stress syndrome. Physical therapists may prescribe specific stretching and strengthening exercises to address muscle imbalances or weaknesses around the lower leg. For example, calf stretches, along with exercises that strengthen the muscles around the shin bone, including the tibialis anterior and posterior, can help to improve stability, reduce strain, and accelerate recovery. Furthermore, a therapist might utilize manual therapies, such as soft tissue massage and joint mobilization, to relieve tension and improve overall tissue health. It’s important to understand that healing from medial tibial stress syndrome, the medical terminology for shin splints, typically requires time and consistency in these types of treatment approaches. Listening to the body’s signals, avoiding overexertion, and carefully progressing back to full activity levels are crucial aspects of ensuring a successful recovery, promoting long-term stability, and preventing relapses.